Abstract
Introduction: Hemorrhagic cystitis (HC) causes significant morbidity following allogeneic hematopoietic cell transplantation (HCT). Reactivation of BK polyoma virus frequently occurs following transplantation and appears to be the most commonly associated factor, although high dose cyclophosphamide, other viruses, and numerous other factors contribute. A higher incidence of BK HC was reported with the use of matched unrelated or cord blood donors compared to HLA-matched siblings (El-Zimaity M, et al. Blood. 2004), however, the intensity of GVHD prevention regimens varied according to cell source complicating interpretation of these data. The effect of HLA-mismatched donors on the incidence of BK HC has been disputed and a large study of mismatched donors detected no association of HC with mismatched compared to matched donors (Giraud G, et al. Bone Marrow Transplant, 2008; Gilis L, et al. Bone Marrow Transplantation, 2014.)
We analyzed a cohort of patients biologically assigned to matched sibling (MSD) or haploidentical family donor (based on presence of a suitable MSD donor) who received identical myeloablative or nonablative conditioning regimens and identical PTCy-based GVHD prevention to directly analyze the association of donor source with HC.
Methods: To evaluate the role of haploidentical vs MSD donor source, we analyzed all patients undergoing haploidentical or MSD HCT at the Levine Cancer Institute between March 2014 and June 2018. Patients received identical myeloablative (BuCy) or nonmyeloablative (Flu/Cy/TBI) conditioning regimens followed by peripheral blood stem cell grafts and identical PTCy-based regimens which included tacrolimus and mycophenolate for GVHD prevention. The cumulative incidence of HC was calculated in a competing risk setting with death from any cause as a competing event. Group comparisons of incidences were determined by a Gray's test. Cox regression was conducted to evaluate risk factors for the development of HC. It was also used to evaluate HC as a time-dependent risk factor for overall survival. Fisher's exact test was used to analyze categorical patient characteristics, and two-sample t-test was employed for continuous variables.
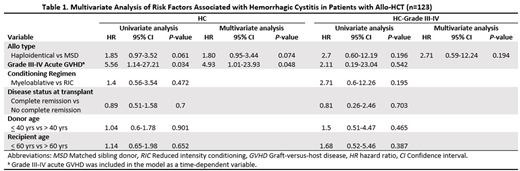
Results: From March 2014 to June 2018, 39 patients (32%) underwent MSD transplantation and 84 patients (68%) received transplants from haploidentical donors. Baseline characteristics were similar except for younger donor age of haploidentical donors (median 40 yrs vs 54 yrs P< .001). The rates of acute GVHD, Chronic GVHD, NRM and overall survival were similar between the two groups. The cumulative incidence of HC was higher in patients who received cells from haploidentical donors when compared to matched related donors (p=0.05). In multivariate analysis of risk factors associated with HC (Table 1), haploidentical donor (HR: 1.80, 95% CI 0.95-3.44, P= .07) and, grade III-IV acute GVHD (HR: 4.93, 95% CI 1.01-23.93 P = .05), were associated with development of HC. 33/53 HC patients (62%) were tested positive for BK virus. The intensity of the conditioning regimen, disease status at transplant, donor and recipient age were not associated with development of HC. For patients who received cells from haploidentical donors, there was a trend towards severe (grade 3-4) HC, but this did not reach statistical significance (HR 2.71, 95% CI 0.59-12.24 P=.19). The incidence of HC was not associated with overall survival (HR 0.58 95% CI 0.3-1.15 P=0.12), even when severe (grade III-IV) HC events were evaluated (HR 1.79 95% CI 0.75-4.3 P=0.19).
Conclusions: In adults undergoing allogenic transplantations using identical conditioning regimens and PTCy based GVHD prevention, the use of a haploidentical donor results in a higher incidence of HC than does a MSD.
Grunwald:Cardinal Health: Consultancy, Membership on an entity's Board of Directors or advisory committees; Forma Therapeutics: Research Funding; Ariad: Consultancy, Membership on an entity's Board of Directors or advisory committees; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Alexion: Consultancy, Membership on an entity's Board of Directors or advisory committees; Medtronic: Equity Ownership; Genentech: Research Funding; Incyte Corporation: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Consultancy, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees; Merck: Consultancy, Membership on an entity's Board of Directors or advisory committees; Janssen: Research Funding. Jacobs:Genentech: Honoraria. Usmani:Abbvie, Amgen, Celgene, Genmab, Merck, MundiPharma, Janssen, Seattle Genetics: Consultancy; Amgen, BMS, Celgene, Janssen, Merck, Pharmacyclics,Sanofi, Seattle Genetics, Takeda: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal